全球COVID-19病例已经有几千万例,死亡人数超过百万。约1%的COVID-19病例患有恶性肿瘤,1其中肺癌占相当大的比例。肺癌患者在感染COVID-19后往往会出现严重的病情,2这突出了准确、迅速诊断COVID-19在肺癌治疗中的重要性。虽然COVID-19诊断参考逆转录聚合酶链式反应(RT-PCR)测试,但胸部CT扫描可以偶然发现COVID-19,这是诊断和监测肺癌的一种重要影像学方式。韩国首尔国立大学医院放射科医学博士Soon Ho Yoon和Jin Mo Goo分享经验,介绍如何通过CT区分肺癌患者的COVID-19肺炎和非COVID-19疾病。
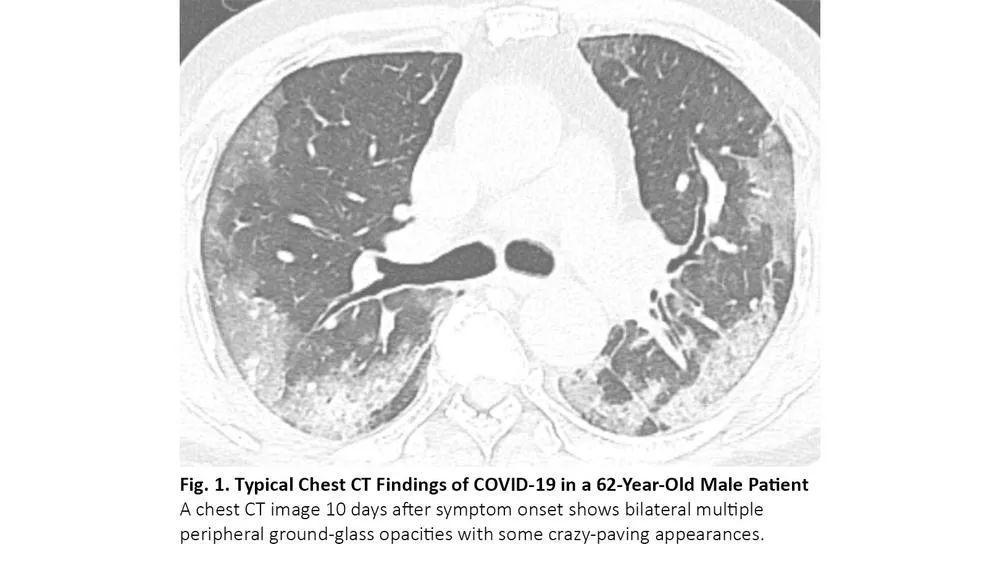
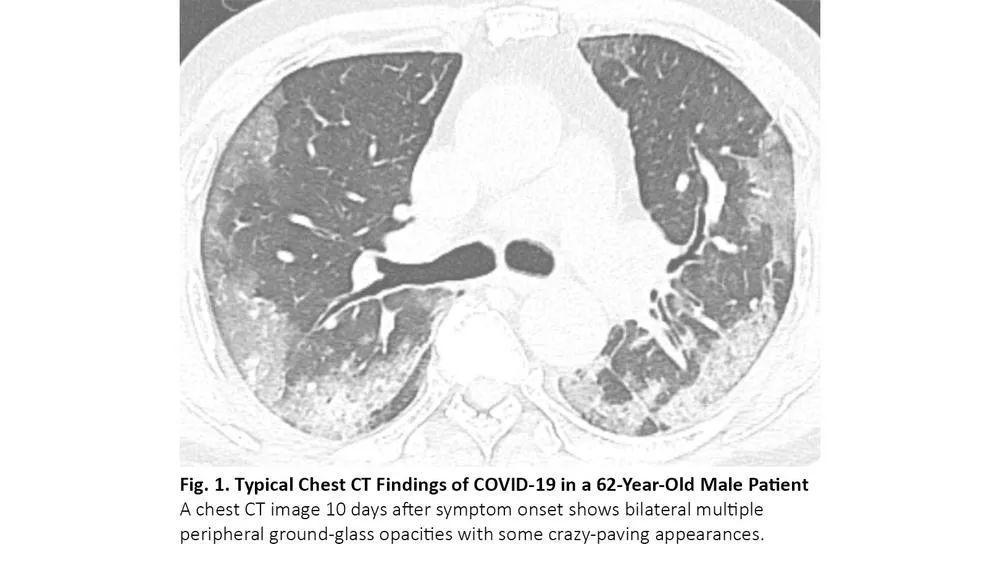
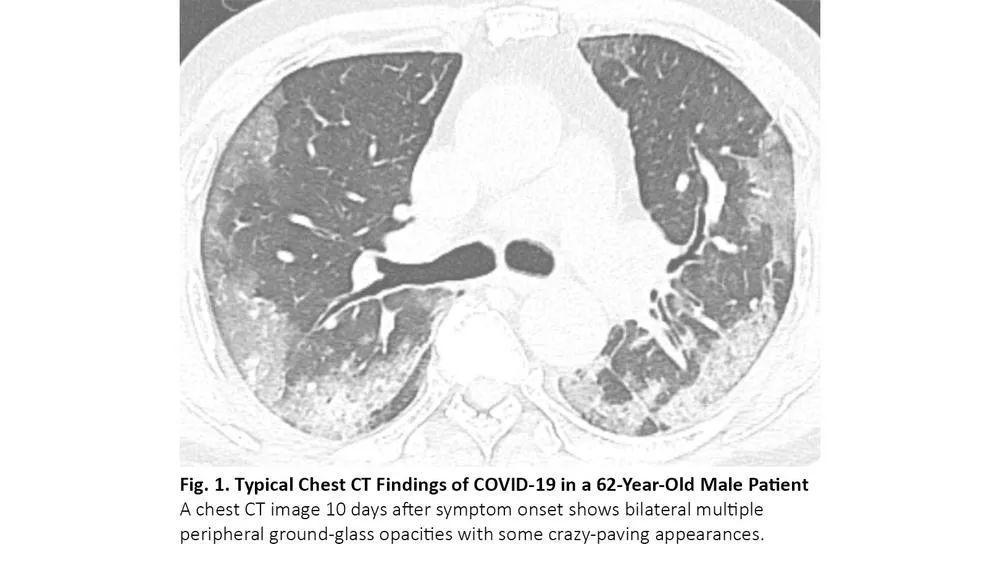
COVID-19患者的肺部CT的典型表现为双侧多发磨玻璃样影,好发于肺周3(图1)。61%~72%的COVID-19患者在症状出现后1周左右有典型CT表现,而非COVID-19患者只有不到10%人群有此类表现。4,5
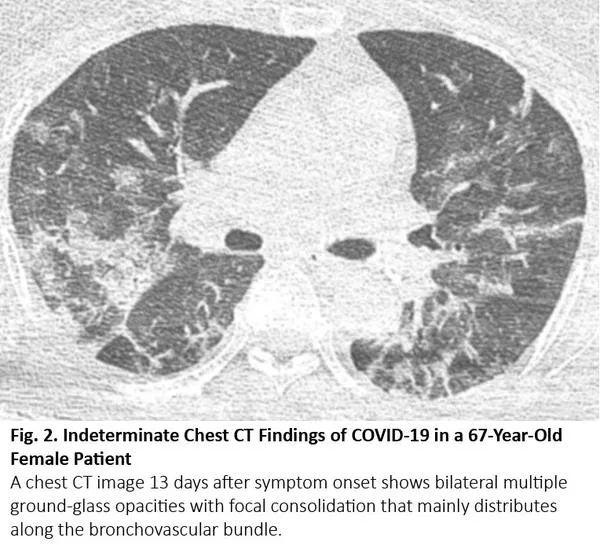
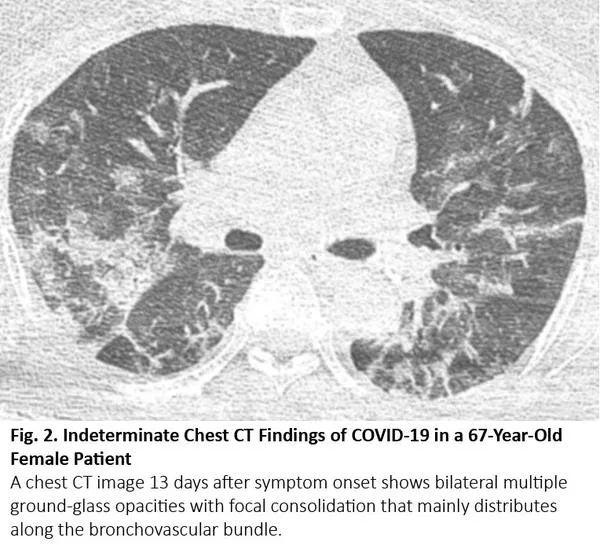
COVID-19的胸部CT可伴有局部的实质化和网状阴影(铺路石征影像表现)或其他组织性肺炎的表现,如反晕征。17% - 20%的COVID-19患者的CT与各种感染性、非感染性肺部疾病(如超敏性肺炎、肺孢子虫肺炎和弥漫性肺泡出血)难以区分(图2)。
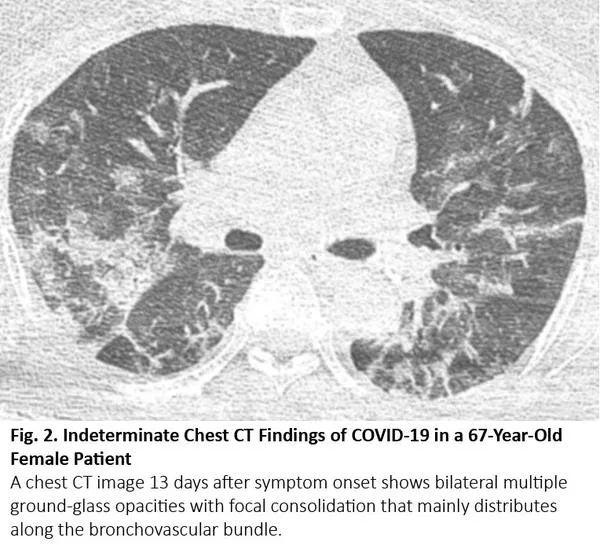
图2. 一位67岁女性患者的胸部CT呈现COVID-19不典型特征
3%~17%的COVID-19患者没有呈现COVID-19的典型CT特征。相当一部分COVID-19患者的CT结果是阴性(没有呈现出COVID-19感染导致的CT异常);阴性CT结果更常见于儿童和无并发症的无症状患者。6症状出现后的CT扫描时机也影响着鉴别和CT异常程度。高达56%的COVID-19患者在症状出现后2天内CT扫描结果正常,7随着症状持续,CT异常程度增加,在COVID-19症状出现后10天左右达到高峰。
胸部CT成像对COVID-19的敏感度为93%,特异性为37%。6随着COVID-19病例的增加,一项研究报告称,胸部CT的特异性提高到约80%,而敏感性仍高于90%。9
感染性、非感染性肺部疾病CT表现与COVID-19类似
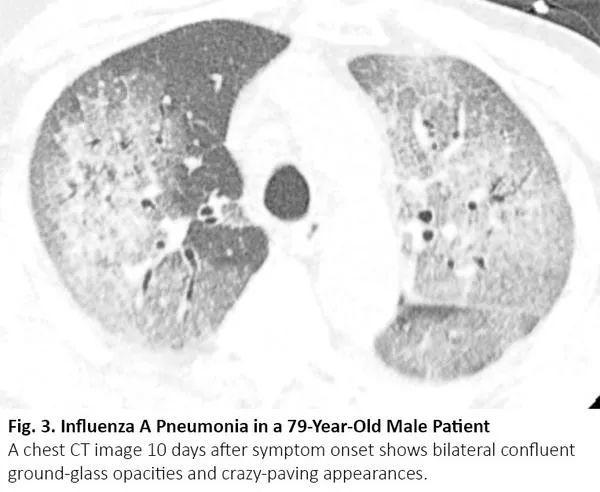
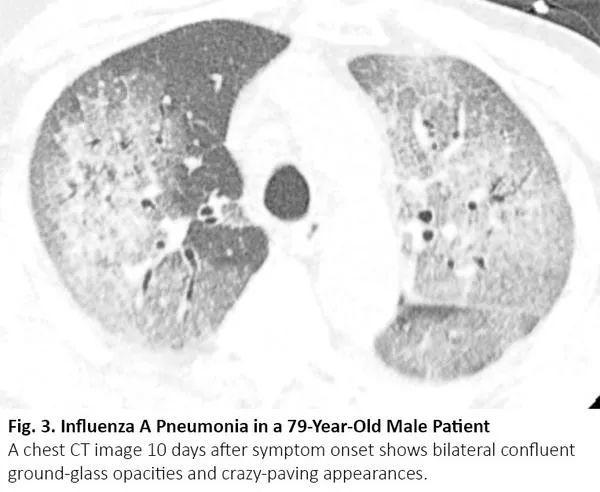
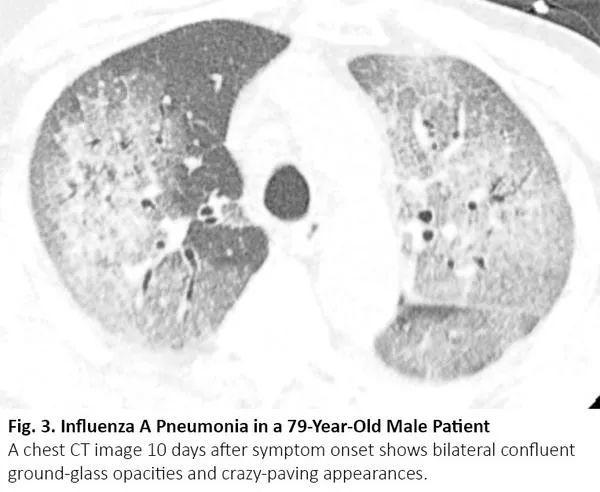
肺癌患者在病程中可能出现与COVID-19类似的CT异常,但这些异常是由于其他原因,如病毒性肺炎、癌症复发和间质性肺病。病毒性肺炎,特别是流感肺炎,在胸部CT上可表现为双侧磨玻璃样影和实性病变,胸部CT上位置分布相似10(图3),秋冬流感高发时,利用放射学检查结果来鉴别二者可能有问题。COVID-19 CT比流感肺炎CT更多见小叶间隔增厚及圆形阴影(典型肺周分布),但肺结节和树芽征相对更少。11
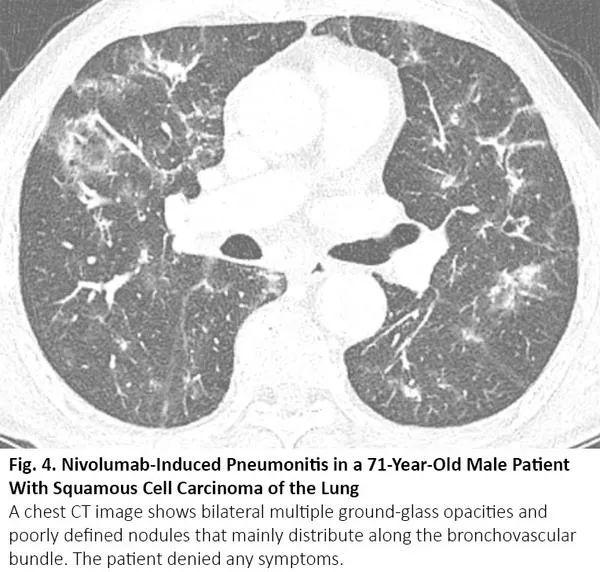
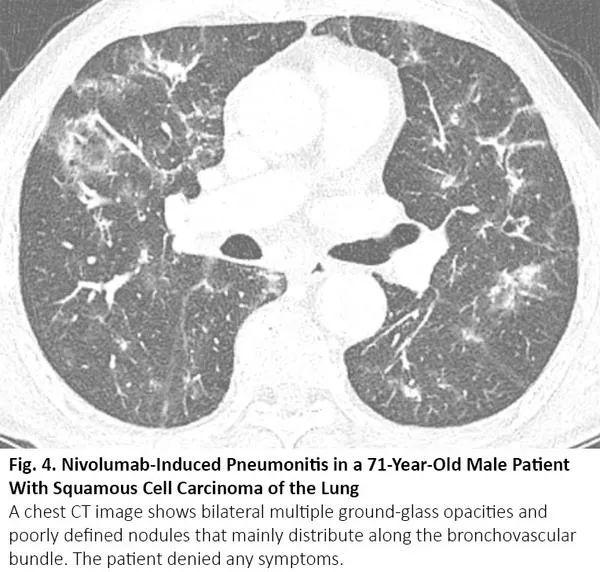
化疗、免疫治疗可引起药物性肺炎,导致CT呈现间质性肺部疾病的影像学表现。12最常见的类型是隐源性机化肺炎,其次是非特异性间质性肺炎、超敏性肺炎和急性间质性肺炎。13其中,隐源性机化肺炎、非特异性间质性肺炎的影像学表现可与COVID-19肺炎相似(图4),反之亦然。14
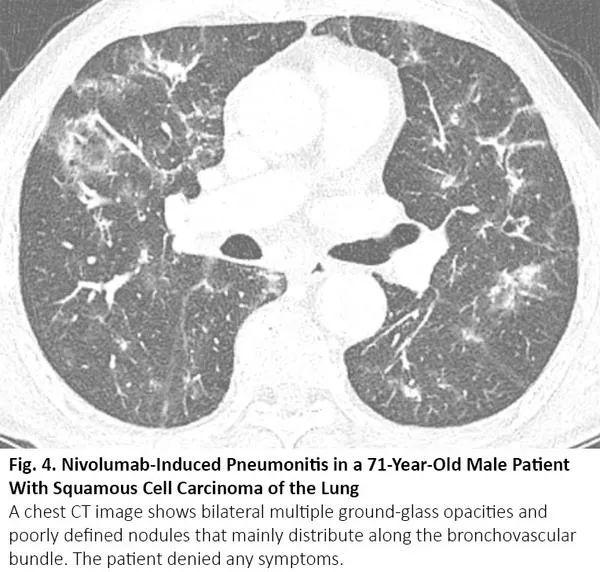
图4. 一位71岁肺鳞癌男性患者出现纳武利尤单抗治疗导致的肺炎
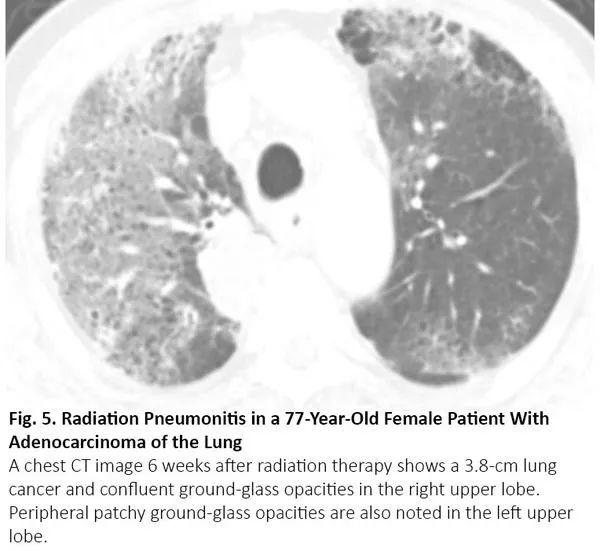
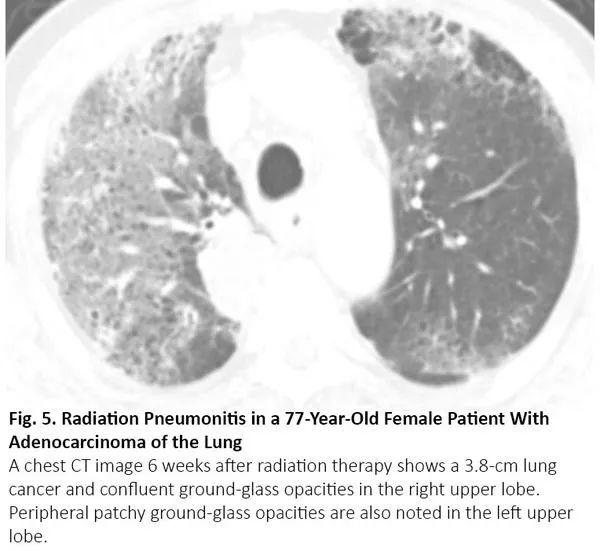
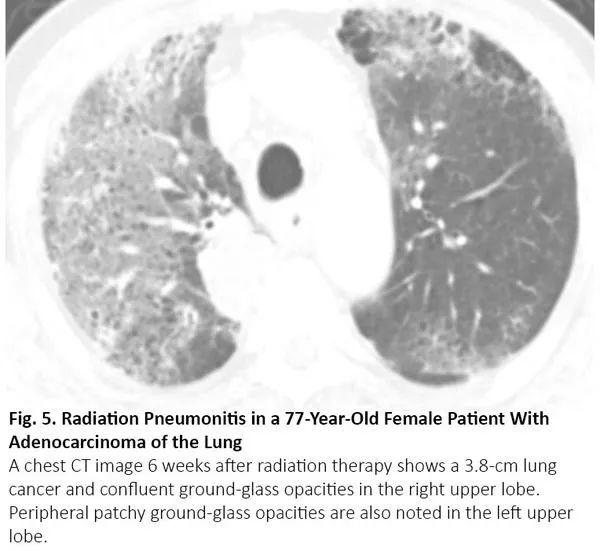
放疗结束后4~12周内可能发生放射性肺炎,有时更晚15。因为放射性肺炎通常发生在照射野,发生于局部,因此在大多数情况下,放射性肺炎与COVID-19肺炎的影像鉴别很简单。然而,当肺炎呈弥漫性分布时,可能无法将放射性肺炎与COVID-19肺炎区分(图5)。
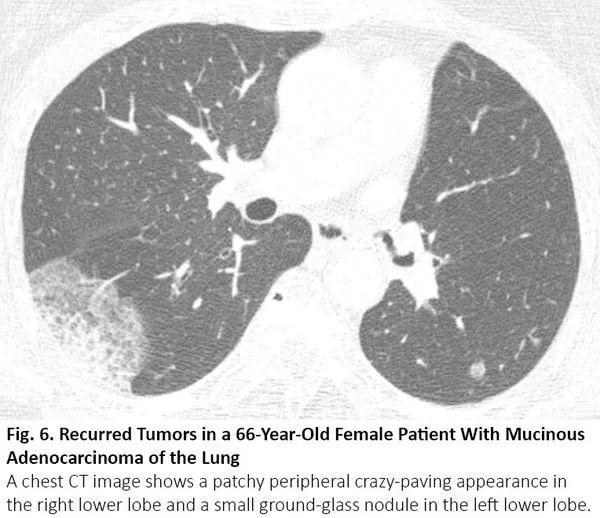
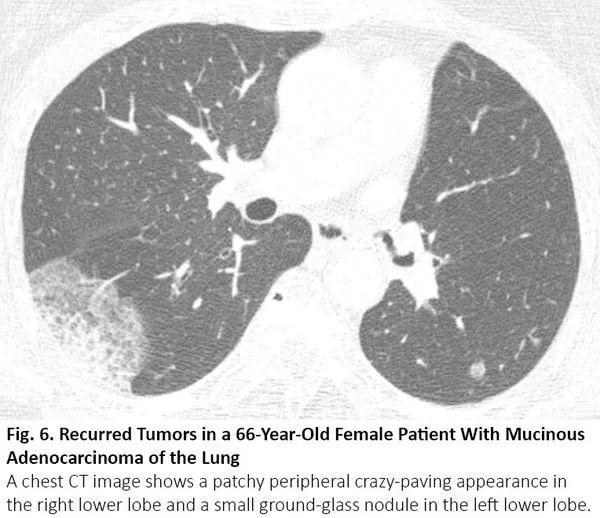
肺癌CT通常表现为结节或肿块,但有时也可表现为空洞。浸润性黏液腺癌是一个著名的例子,可呈现实性病变,伴或不伴磨玻璃样影,类似肺炎。腺癌的特定亚型,包括伏壁式、腺泡型和乳头型为主的腺癌,CT图像可呈现毛玻璃样阴影的区域。16当这些病变发生在肺部多处,其胸部CT可能与COVID-19有相似(图6)。如果既往的胸部CT显示这些病变已经持续存在,则可以与COVID-19区分。
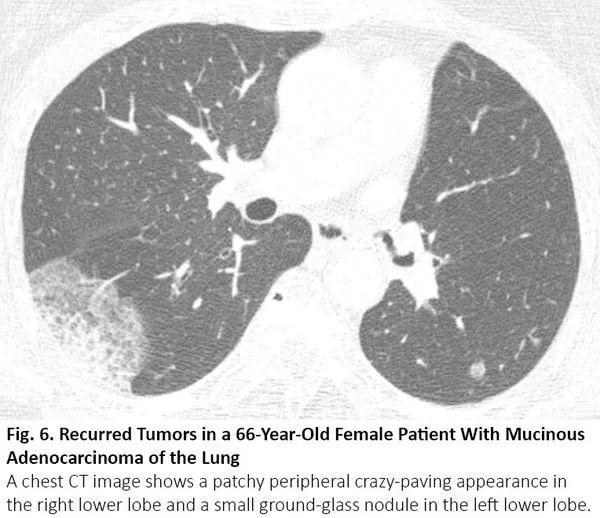
图6. 一位66岁粘液性肺腺癌患者肿瘤复发后的胸部CT
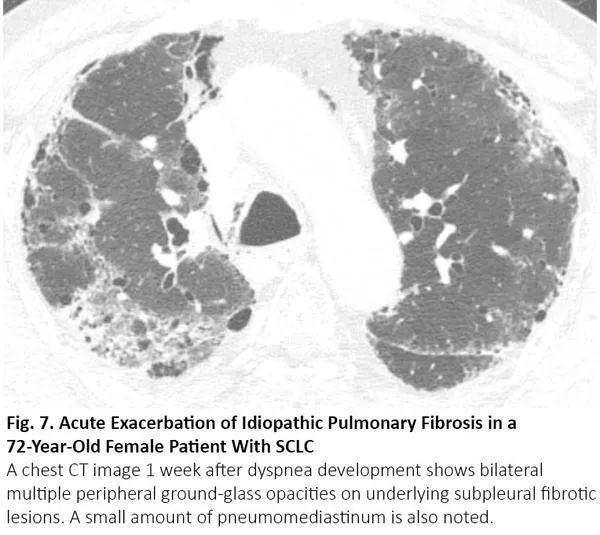
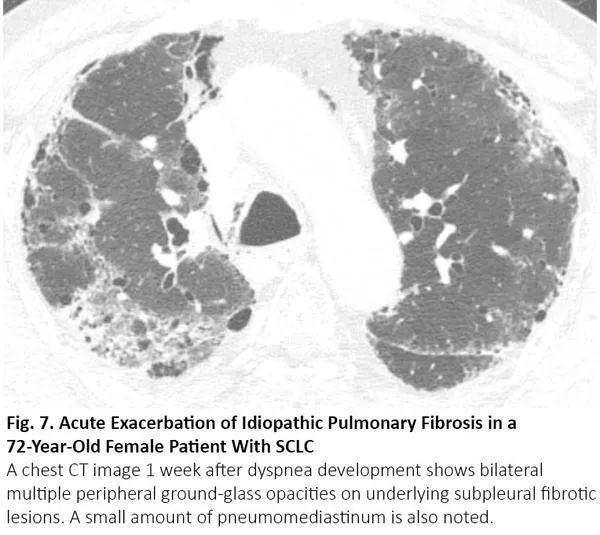
吸烟增加罹患肺癌和特发性肺纤维化(IPF)的风险,特发性肺纤维化患者罹患肺癌的风险会增加。当患者接受手术或放疗时,若特发性肺纤维化急性加重,CT可呈现双肺弥漫性或外周磨玻璃影,17与COVID-19肺炎相同(图7)。
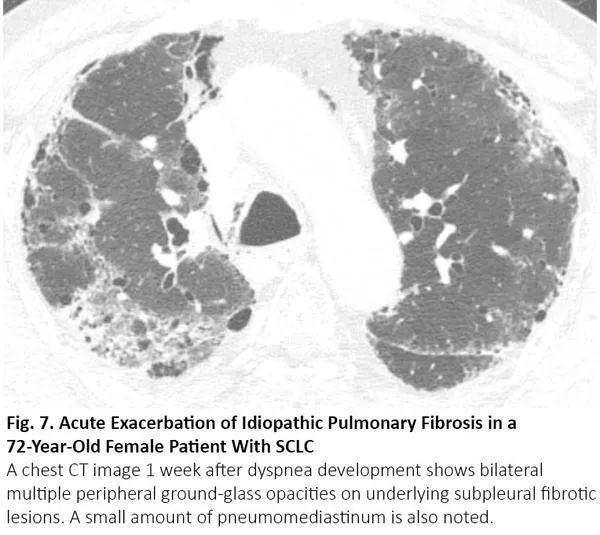
图7. 一位72岁的小细胞肺癌女性患者出现特发性肺纤维化急性加重
总而言之,COVID-19肺炎可导致肺癌患者病情恶化,COVID-19 CT与肺癌治疗过程中的胸部CT有相似之处。仅凭胸部CT很难区分COVID-19肺炎和非COVID-19疾病,临床医生应谨慎评估,利用逆转录聚合酶链反应检测来确认是否存在COVID-19感染。
1.Liang W, Guan W, Chen R, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335-337.
2.Luo J, Rizvi H, Preeshagul IR, et al. COVID-19 in patients with lung cancer. Ann Oncol. 2020. [Epub ahead of print].
3.Simpson S, Kay FU, Abbara S, et al. Radiological Society of North America Expert Consensus Statement on Reporting Chest CT Findings Related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA. Radiology: Cardiothoracic Imaging. 2020;2(2):e200152.
4.Ciccarese F, Coppola F, Spinelli D, et al. Diagnostic accuracy of North America Expert Consensus Statement on Reporting CT Findings in Patients with Suspected COVID-19 Infection: an Italian single center experience. Radiology: Cardiothoracic Imaging. 2020;2(4):e200312.
5.Prokop M, van Everdingen W, van Rees Vellinga T, et al.. CO-RADS: a categorical CT assessment scheme for patients suspected of having COVID-19 - definition and evaluation. Radiology. 2020;296(2):E97-E104.
6.Kim H, Hong H, Yoon SH. Diagnostic performance of CT and reverse transcriptase-polymerase chain reaction for coronavirus disease 2019: a meta-analysis. Radiology. 2020. [Epub ahead of print].
7.Bernheim A, Mei X, Huang M, et al. Chest CT findings in Coronavirus Disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020;295(3):200463.
8.Pan F, Ye T, Sun P, et al. Time course of lung changes at chest CT during recovery from Coronavirus Disease 2019 (COVID-19). 2020;295(3):715-721.
9.Falaschi Z, Danna PSC, Arioli R, et al. Chest CT accuracy in diagnosing COVID-19 during the peak of the Italian epidemic: a retrospective correlation with RT-PCR testing and analysis of discordant cases. Eur J Radiology. 2020. [Epub ahead of print].
10.Agarwal PP, Cinti S, Kazerooni EA. Chest radiographic and CT findings in novel swine-origin influenza A (H1N1) virus (S-OIV) infection. Am J Roentgenology. 2009;193(6):1488-1493.
11.Liu M, Zeng W, Wen Y, Zheng Y, Lv F, Xiao K. COVID-19 pneumonia: CT findings of 122 patients and differentiation from influenza pneumonia. Eur Radiol. 2020. [Epub ahead of print].
12.Ryu JH. Chemotherapy-induced pulmonary toxicity in lung cancer patients. J Thorac Oncol. 2010;5(9):1313-1314.
13.Nishino M, Ramaiya NH, Awad MM, et al. PD-1 inhibitor-related pneumonitis in advanced cancer patients: radiographic patterns and clinical course. Clin Cancer Res. 2016;22(24):6051-6060.
14.Artigas C, Lemort M, Mestrez F, Gil T, Flamen P. COVID-19 pneumonia mimicking immunotherapy-induced pneumonitis on 18F-FDG PET/CT in a patient under treatment with nivolumab. Clin Nucl Med. 2020;45(8):e381-e382.
15.Choi YW, Munden RF, Erasmus JJ, et al. Effects of radiation therapy on the lung: radiologic appearances and differential diagnosis. Radiographics. 2004;24(4):985-997, 998.
16.Austin JH, Garg K, Aberle D, et al. Radiologic implications of the 2011 classification of adenocarcinoma of the lung. Radiology. 2013;266(1):62-71.
17.Kim DS, Park JH, Park BK, Lee JS, Nicholson AG, Colby T. Acute exacerbation of idiopathic pulmonary fibrosis: frequency and clinical features. Eur Respir J. 2006;27(1):143-150.
(来源:《肿瘤瞭望》编辑部)
本篇文章来源于微信公众号: ioncology